Poster Presentation 33rd ASM of the Australian & New Zealand Bone & Mineral Society 2023
Atypical femur fracture… What to do AFFTER Teriparatide? (#255)

 Atypical femur fracture… What to do AFFTER Teriparatide?
Atypical femur fracture… What to do AFFTER Teriparatide?
We present the case of Ms JA, a 73-year-old lady who developed bilateral atypical femur fractures that were treated conservatively with Teriparatide.
JA is originally from the UK and lives between Sydney and Southeast England. She lives with her husband, is a non-smoker, drinks 20g of alcohol per day and is generally fit and well for her age.
In addition to osteoporosis, her medical history includes a meningioma that was resected in 2012.
This was complicated by growth hormone deficiency which is treated with daily Somatropin 0.2 mg subcutaneous at night. She is also treated for hypertension, hypercholesterolemia and glaucoma. Her other medications include Ramipril 10mg, Pravastatin 10mg and vitamin D 2000 units daily.
In terms of her long-standing osteoporosis, JA had a minimal trauma distal radius fracture in 2007 and again in 2015, and compression fracture of T7 in 2010.
She commenced treatment with alendronate in 2009. At the time her spine T-score was -3.2 and total hip T-score was -1.5. In 2012 due to issues with gastrointestinal tolerability, she was changed to Denosumab 60mg six monthly injections.
In 2019, after 11 years of continuous anti-resorptive treatment, she developed bilateral thigh pain on walking. Her symptoms worsened progressively over the next 12-18 months with walking becoming difficult due to pain.
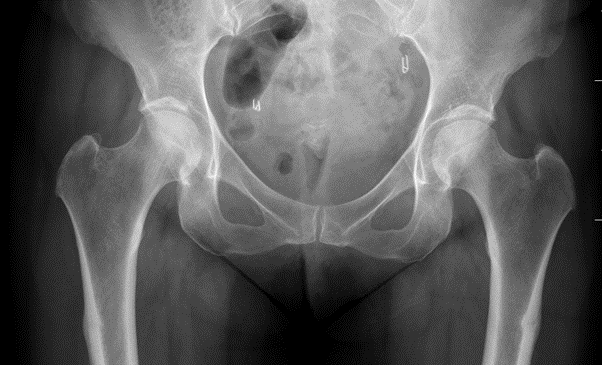
In October 2020 when living in the UK, X-ray demonstrated bilateral femoral sub trochanteric cortical thickening with a subtle fracture line on the left.
She was subsequently diagnosed with having bilateral atypical femur fractures (AFFs) and Denosumab was ceased with her final dose being in April 2020.
Fig 1. X-ray October 2020
JA declined surgical management with prophylactic intramedullary nail insertion. She was managed by a Rheumatologist and Teriparatide and Strontium ranelate were considered. She did not meet NICE criteria for Teriparatide, nor was her treating team successful in gaining approval for special access funding. Strontium ranelate was deemed too high risk in terms of cardiovascular risk in the setting JA’s history of hypertension and hyperlipidaemia.
Consequently, she did not receive any immediate treatment, but her pain improved. By 12 months after her last Denosumab dose, she was walking up to 10,000 steps per day but still experienced a dull ache following more intense physical activity.
She returned to Australia and plain film from February 2021 (fig 2) demonstrated ongoing cortical thickening of the lateral cortex of both femurs, but fracture lines had improved.
Fig 2. X-rays February 2021 and ten months post Denosumab cessation.
March 2021 she was reviewed by the St Vincent’s bone and calcium clinic.
DEXA scan demonstrated only slight reduction in bone density since cessation of Denosumab and spine T-score was -2.2 and hips scores ranged from -1.0 to -1.4.
As there was clinical and radiological improvement of the AFFS and bone density was relatively stable, conservative management with ongoing surveillance continued.
In May she was admitted with back pain and imaging demonstrated further vertebral compression fracture of T9.
Due to her high risk of further fractures, treatment was reinstated.
Romosuzomab was discussed but due to the paucity of data in atypical femur fractures, daily Teriparatide 20mcg injections were commenced in June 2021.
She returned back to the UK and hypercalcaemia was noted on routine bloods in August 2021 up to 2.90mmol/L. Medical advice in the UK was to decrease the Teriparatide to 20mcg second daily and cease her calcium supplement.
JA has continued on second daily Teriparatide and serum calcium has normalised and CTX and P1NP remain elevated consistent with Teriparatide treatment.
A CT scan from June 2022 demonstrated complete healing of the prior atypical femur fractures. Her bone density continued to decrease despite the Teriparatide which can be attributed to cessation of Denosumab and that Teriparatide was only alternate days dosing. Discussion: This case raises several complex clinical issues, including the nature, incidence and management of atypical femur fractures, specifically conservative management, and the use of Teriparatide rather than prophylactic intramedullary nails.
A JCEM review of case reports and cohort studies supports that Teriparatide may assist healing post atypical femur fracture, especially if surgically managed but the efficacy in non-surgically managed AFFs is less clear [i].
The authors recognise the reported data is not sufficient for an evidence-based recommendation of the use of teriparatide to accelerate healing of AFF. A high-quality RCT on the use of teriparatide (or abaloparatide) in healing of AFFs would aid clinical decision making, however of yet, such a study has not been completed.
This case also raises the very challenging clinical question of ongoing osteoporosis management following AFF for patients who remain at high risk of osteoporotic fractures.
Continuation of anti-resorptive treatment is associated with increased risk of contralateral AFF, however patients remain at high risk of further osteoporotic fracture.
Teriparatide is often recommended after atypical femur fracture and decreases risk of fragility fracture, however currently there are no guidelines for consolidation anti-resorptive treatment and expert opinion is recommended[ii]. Currently there is minimal data reviewing Romosozumab post AFF but this will likely change in coming years.
Managing side effects of Teriparatide, including hypercalcaemia is also raised. Although this is a usually a mild side-effect that does not impact treatment, there have been rare cases of severe hypercalcaemia causing acute renal failure[iii]. Finally, and quite specific to this case, is if her growth hormone deficiency, even if treated, contributed to her osteoporosis and development of atypical femur fractures. References:
[i] van de Laarschot, Denise M., et al. "Medical management of patients after atypical femur fractures: a systematic review and recommendations from the European Calcified Tissue Society." The Journal of Clinical Endocrinology & Metabolism 105.5 (2020): 1682-1699.
[ii] Bégin, Marie‐Josée, et al. "Fracture risk following an atypical femoral fracture." Journal of Bone and Mineral Research 37.1 (2022): 87-94.
[iii] Karatoprak, Cumali, et al. "Severe hypercalcemia due to teriparatide." Indian journal of pharmacology 44.2 (2012): 270.